-
Phone
1300 17 44 97
-
Fax
02 8580 4867
-
-
Correspondence
Suite 1404, Level 14
St Vincent’s Private Hospital
406 Victoria Street
Darlinghurst NSW 2010
MRI-Guided Focussed Ultrasound is currently used to treat conditions such as:
Essential and dystonic tremor usually cause shaking in the hands but can also cause shaking in the legs, the head and the voice. Medications are sometimes effective for tremor but only around half of people obtain significant benefit. Essential and dystonic tremor often gradually worsen over the years.
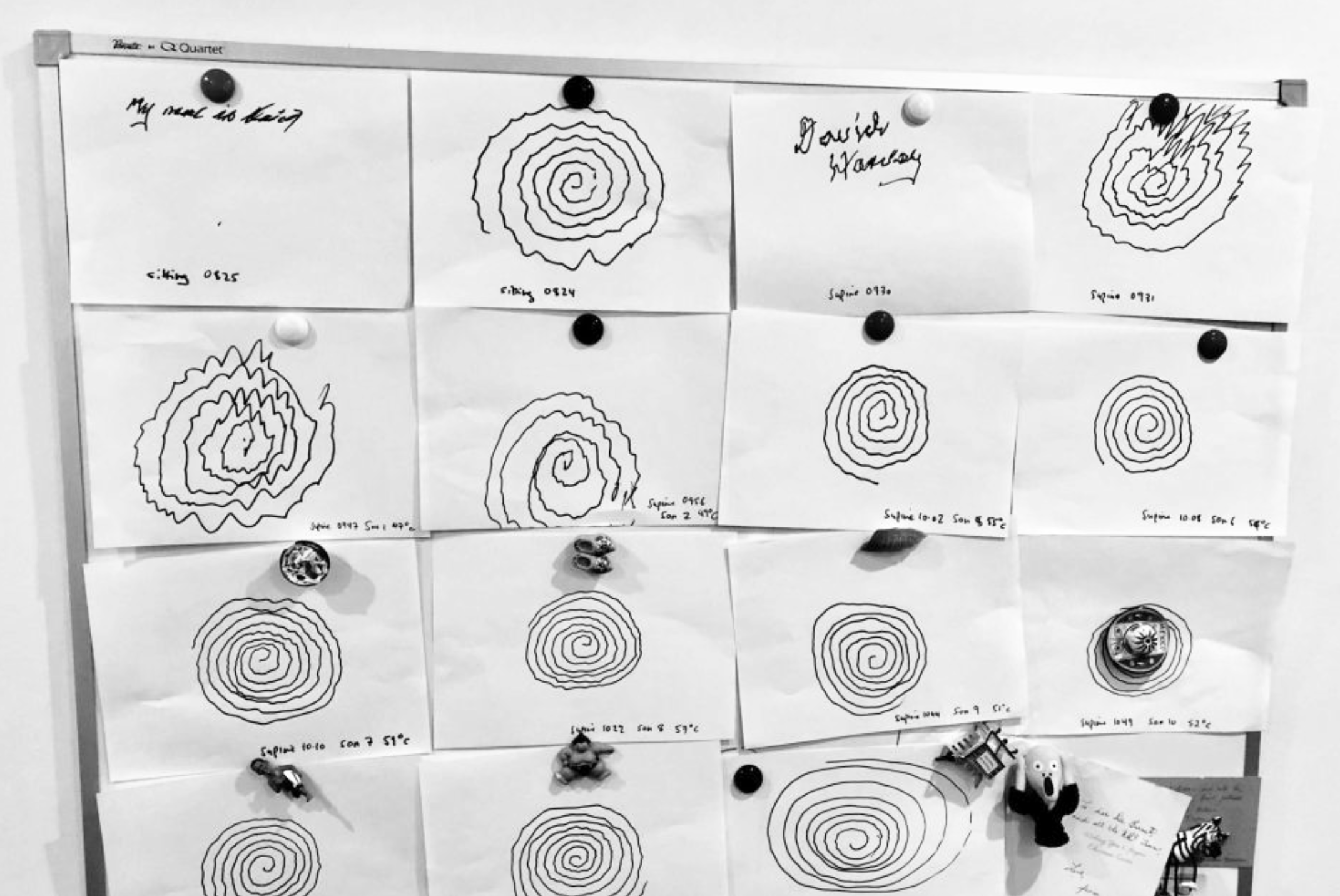
Tremors can affect quality of life and can impede people from eating, drinking and looking after themselves. In addition they can be embarrassing and in some cases can lead to social isolation which in turn can lead to depression. One of the messages we hear time and again from patients with tremor is that whilst others (including well meaning doctors) can sometimes say “it’s just a tremor”, but for the person experiencing the tremor it can be associated with a major reduction in quality of life.
This is a new way of performing thalamotomy that does not require incisions, any holes to be drilled in the head, or any probes to be inserted.
During the MRgFUS thalamotomy procedure, the patient remain fully conscious. A stereotactic head frame is placed on the head with local anaesthetic and the patient lies in the MR scanner. If required some sedation can be given to help maximise comfort and relaxation during the MRI and procedure.
The focussed ultrasound sends 1024 individual ultrasound beams through the brain that intersect at a single point in the thalamus and can destroy the tremor causing cells. This can all be monitored on the MRI and by repeatedly checking the patient and their tremor until the tremor has been adequately treated.
When it is over there is an immediate and significant reduction in tremor.

Most patients experience a significant improvement to their tremor through the treatment process.
Some side-effects have been reported, including numbness in the face or hand and gait disturbance. In most cases these are mild and temporary, but they can be ongoing in some patients.
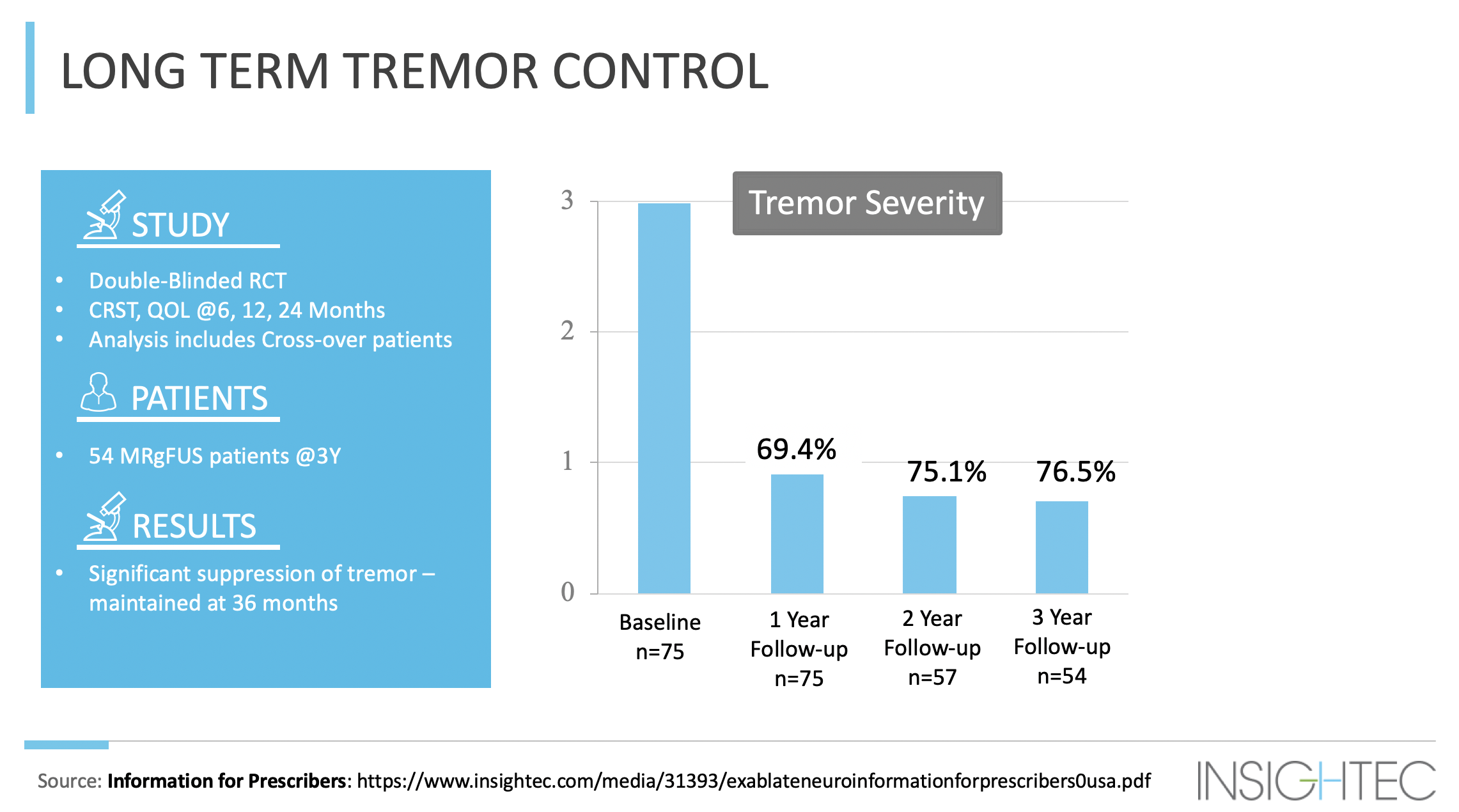
MRgFUS is a relatively new technology and very long term outcomes are not yet available. Current studies stretch to 3-4 years of outcome. The indications thus far suggest that the vast majority of patients will have durable good effect on their tremor by this procedure.
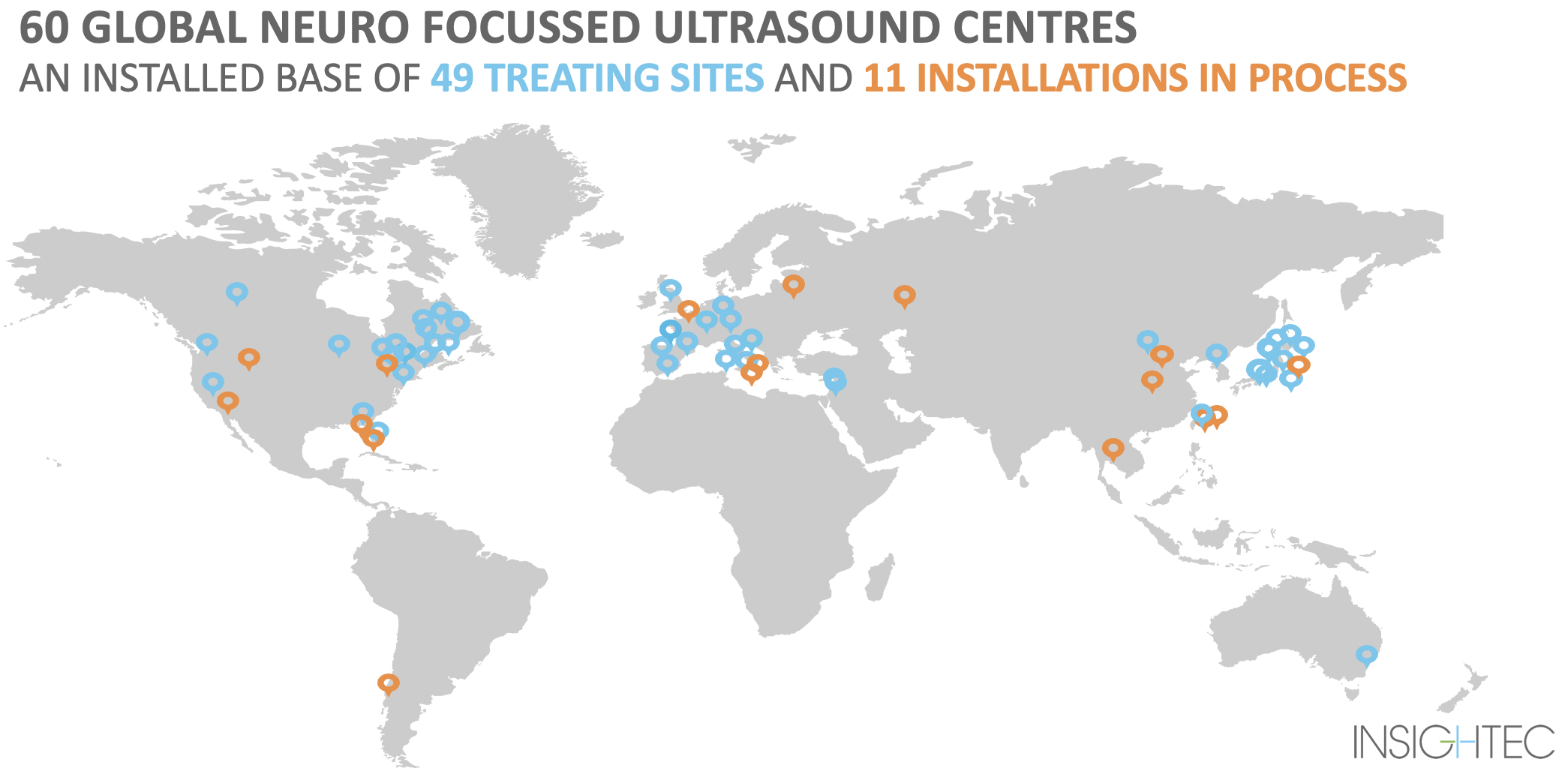
The team at St Vincent’s in Sydney is the first group to provide this treatment in Australia, with the St Vincent’s MRI-Guided Focussed Ultrasound programme being one of only a few in the Southern Hemisphere. Dr Jonker has undertaken visits to a number of overseas centres including Charlottesville, USA, Tokyo, Japan and Seoul, South Korea.
This cutting-edge technology is taking off with over 2,000 treatments performed worldwide, and an increasing number of centres introducing this procedure around the world.
You can contact our office by phone, email or via our website to register your interest in this treatment.
You will be contacted by our practice nurse to briefly discuss the procedure and arrange an assessment if suitable.
The assessment process is multi-faceted and includes the following appointments at St Vincent’s, Sydney –
The results from your consultations and scans are assessed by a dedicated team which comprises of a neurologist, neurosurgeon, neuro-radiologist, movement disorder nurse, and potentially psychologist and other allied health members. In general the assessment will include:
Once the assessment and tests are completed and the results have reviewed, recommendations are discussed with the patient. Further discussions can take place over the phone with our practice nurse or in a face-to-face consultation with the neurologist to answer any queries and finalise the details of your procedure. If the decision is to proceed with treatment, a date for admission and treatment will be arranged.

We accept referrals from interstate and overseas and the above process can be tailored to the individual patient’s situation.
No, these must be done at St Vincent’s Hospital. Specialised scans are done and they will later be used in the treatment process.
Consultations with the neurologist and neurosurgeon take place in their consulting suites at St Vincent’s Clinic or St Vincent’s Private Hospital and are billed at the standard specialist rates.
The assessment process includes dedicated CT and MRI scans, both of which are completed at St Vincent’s Hospital. These are done free of charge for patients with a valid Medicare card.
At this stage medicare does not have reimbursement for the MRgFUS procedure. This is a new procedure so there may be some rebates available in the future, but there is no set time frame for this.
The focussed ultrasound treatment is currently reimbursed in Japan, Italy, Germany, Switzerland, Israel and USA (Medicare covered benefit in 25 states) as of 2019.
Yes, there are usually two nights in hospital, one before the procedure and one after the procedure.
We recommend that you can recommence driving 2 weeks after the procedure. You can travel home, including air travel, within a few days to a week after the procedure.
We are currently doing MRI brain at 3 months postoperatively and there is an assessment of tremor performed at 1 month, 3 months, 6 months and 12 months and then annually thereafter.
Treatments for tremor range from no treatment for very mild cases, through to medications and certain neurosurgical procedures such as thalamotomy and deep brain stimulation.
Medications such as beta-blockers, some anti-seizure medications and some anti-anxiety drugs can be trialled. The side effects vary depending on the medication but can include fatigue or drowsiness. About 50% of people will get some reduction in tremor though the side effects can be limiting.
Thalamotomy is a neurosurgery procedure where a small hole is drilled into the skull and a tiny probe inserted into a part of the thalamus which is containing cells that cause or drive the tremor. These cells can then be destroyed leading to alleviation or complete resolution of the tremor. As with all neurosurgery procedures it carries some risks including bleeding and infection, and a small risk of paralysis or other neurological problems as well as the possibility of other rare problems.
Deep brain stimulation involves drilling a small hole in the head and inserting a permanent electrode into the thalamus or other region causing tremor. This is then connected via a wire to a pacemaker box located in the chest region. It carries some of the same risks as open thalamotomy but also carries risks related to the hardware such as hardware infection. The pacemaker box can be rechargeable or fixed cell and generally will need replacement sometime between 3 and 15 years depending on which model is used.